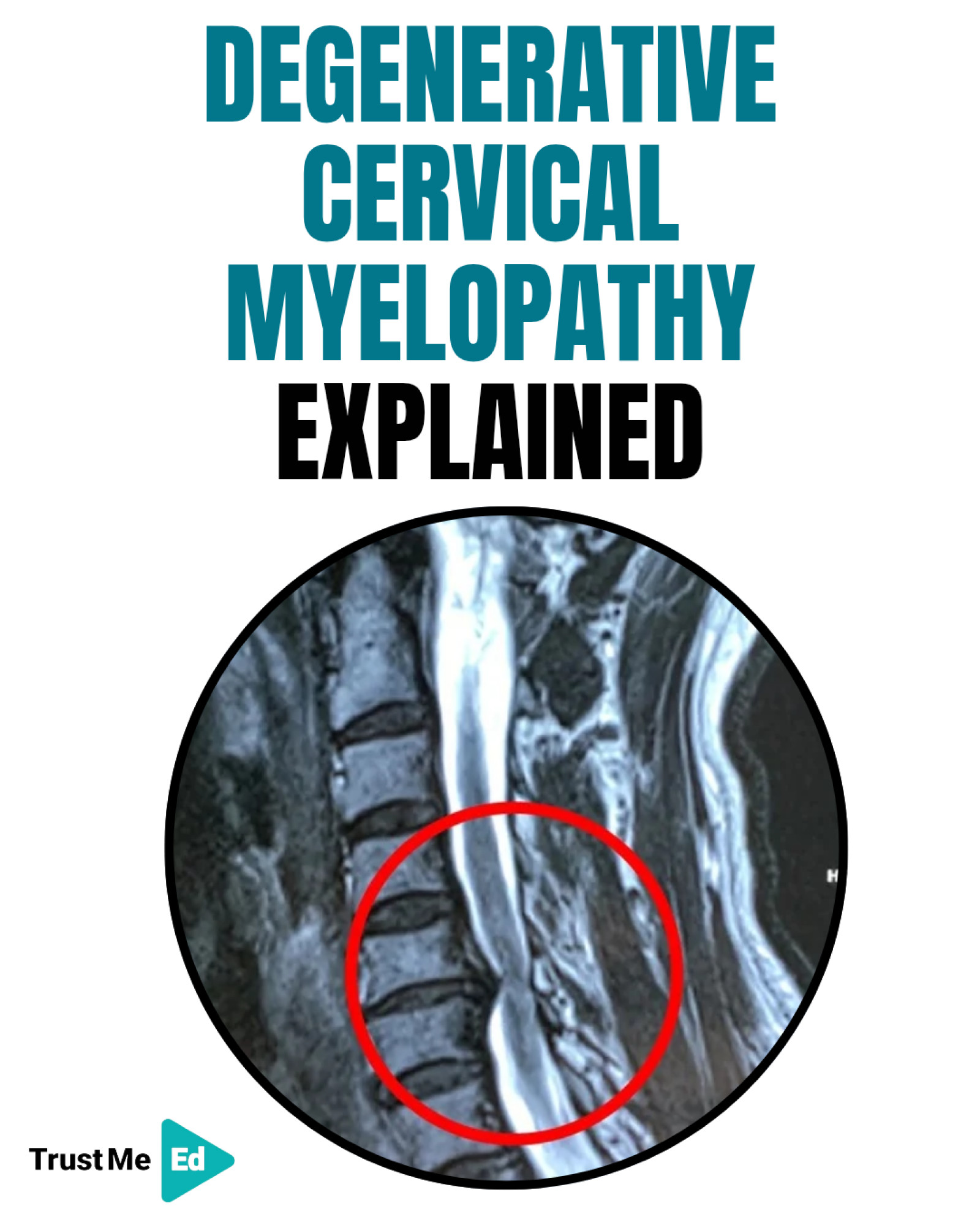
Understanding Degenerative Cervical Myelopathy
What Is Degenerative Cervical Myelopathy?
DCM is a condition where age-related changes in the cervical spine begin to compress or irritate the spinal cord.
Think of it as a “slow-motion spinal cord injury” caused not by trauma, but by gradual wear and tear.
DCM affects roughly 2% of adults, especially those over 50.
If you want to learn more about this topic, you can watch Andy Coombs's lecture here:
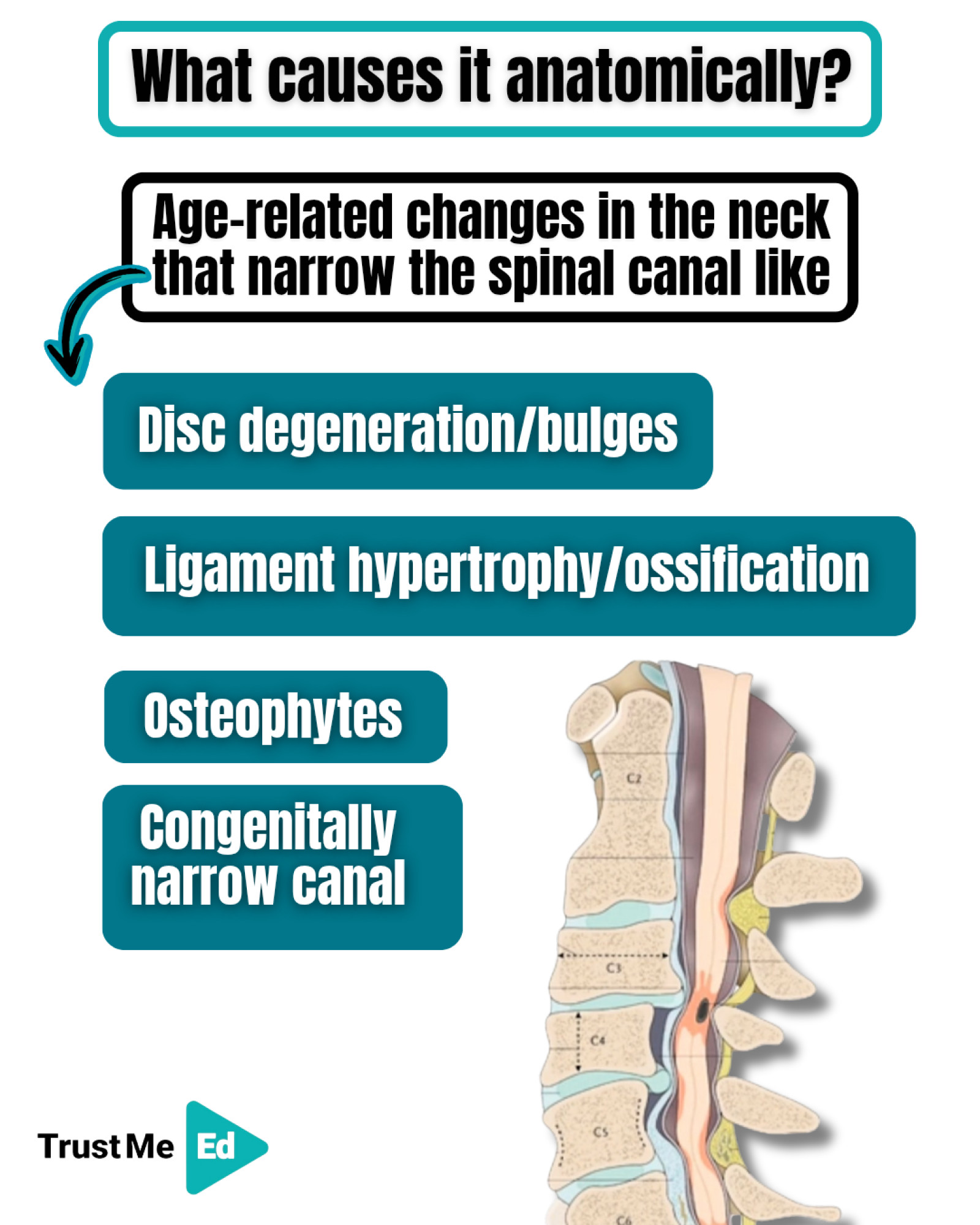
Why does DCM occur?
As we age, structures in the spine change. These changes are often normal—but in some people, they start narrowing the spinal canal and pressuring the spinal cord.
Common Causes Include:
1. Degenerative Disc Changes
The discs may bulge or lose height with age, reducing space around the cord.
2. Osteophytes (Bone Spurs)
Extra bone forms around joints, which can push into the canal.
3. Ligament Thickening
Two main ligaments—the ligamentum flavum and posterior longitudinal ligament—may thicken, buckle, or ossify, further narrowing the space.
4. Congenital Narrow Canal
Some people are simply born with a smaller spinal canal, making them more vulnerable.
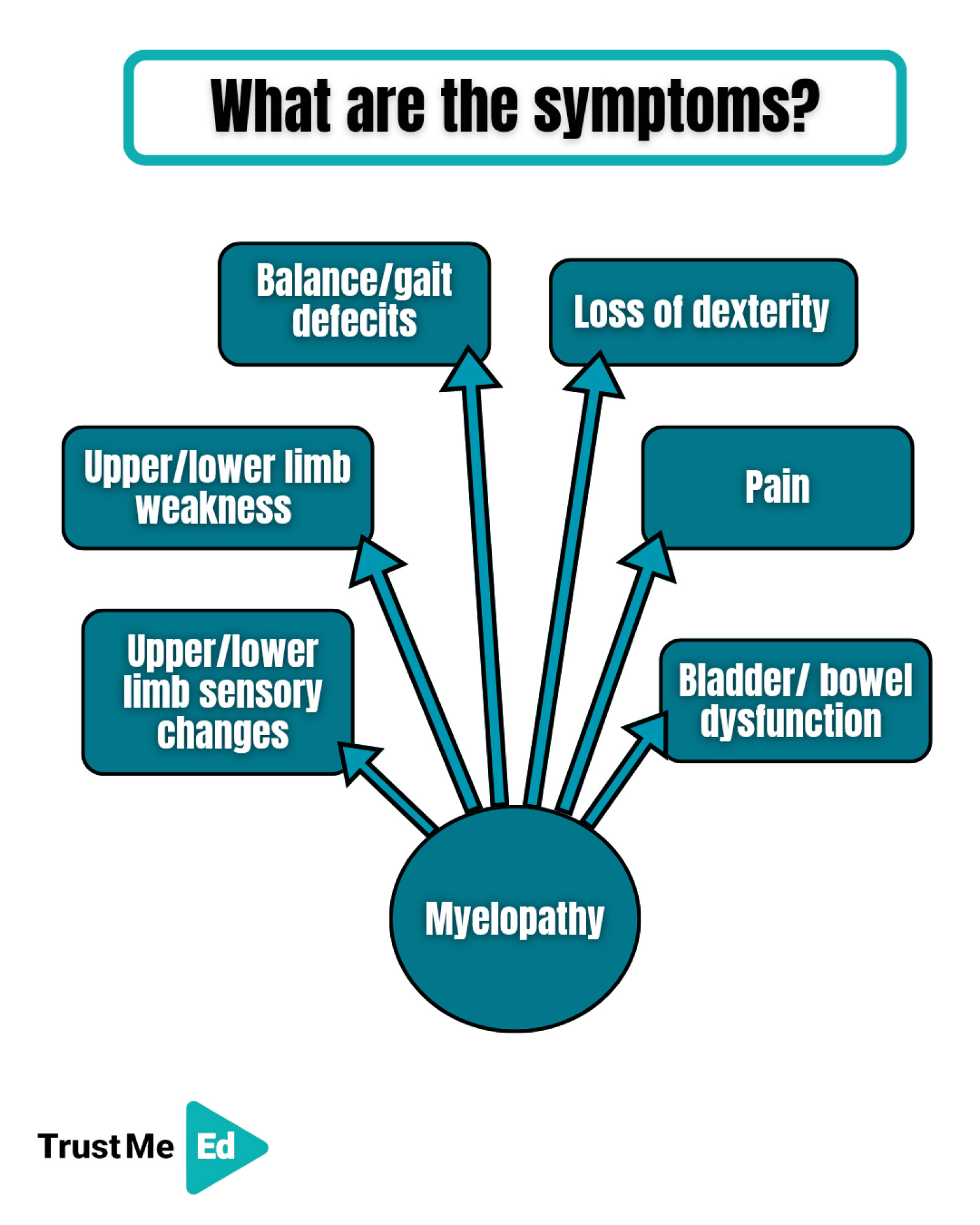
What are symptoms of degenerative cervical myelopathy?
DCM typically develops slowly, often over months or years. Symptoms may come and go, making it tricky to recognise.
1. Upper/lower limb sensory changes
2. Upper/lower limb weakness
3. Balance/ gait defecits
4. Loss of dexterity
5. Bladder/bowel dysfunction
6. Pain

What are the key physical tests for DCM?
1. Tromner’s Test
Flick upward on the patient’s fingertips.
A positive sign shows thumb and finger flexion.
It is more sensitive than Hoffmann’s for DCM.
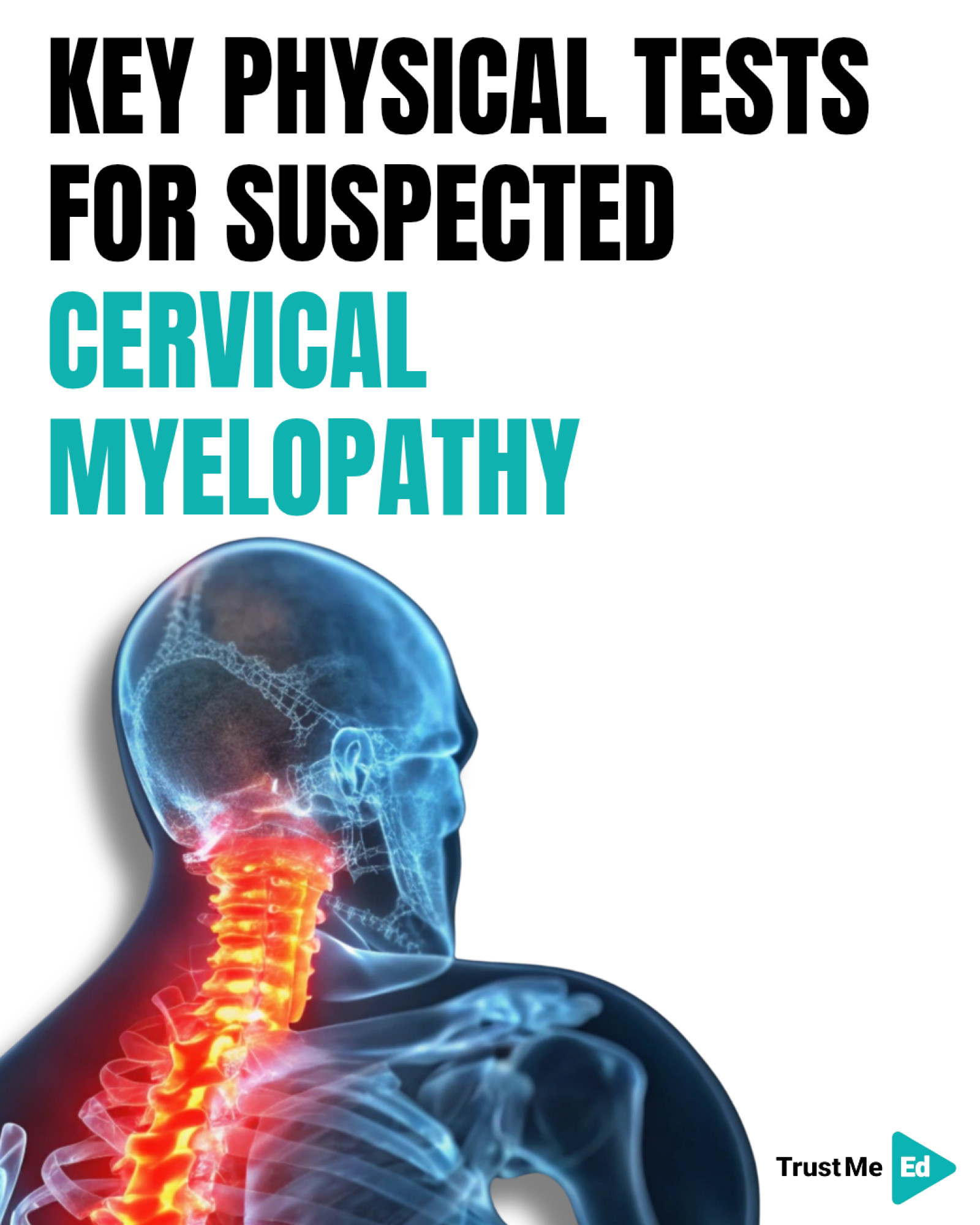
2. Babinski Sign
Stroking the sole of the foot leads to big toe extension.Suggests corticospinal tract involvement.
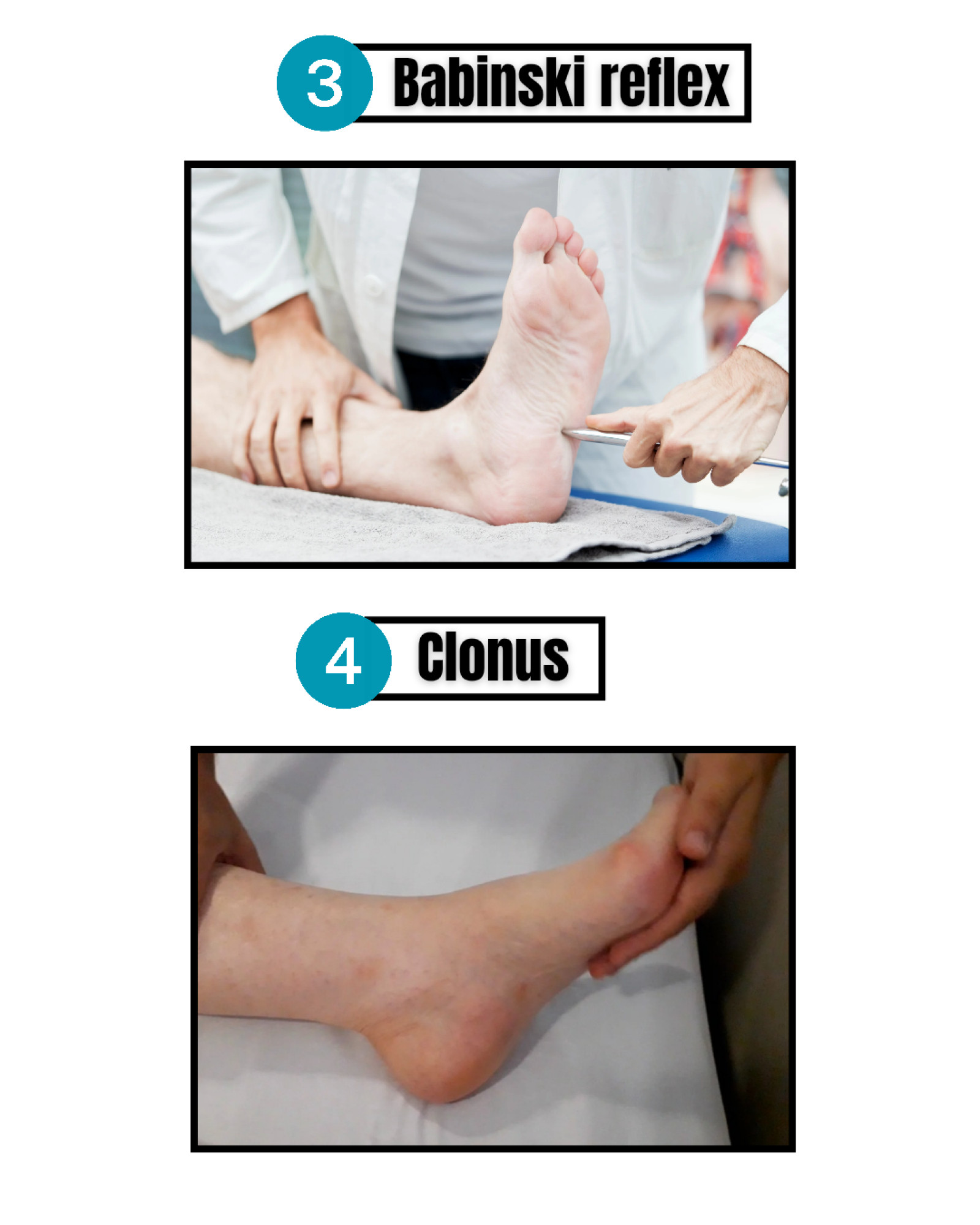
3. Clonus
Repeated rhythmic contractions of the ankle when quickly dorsiflexed. Strong indicator of upper motor neuron dysfunction.
4. Hyperreflexia
One of the hallmark signs of myelopathy.
Because the spinal cord pathways are disrupted, the usual inhibitory control over reflexes is reduced.
You may observe:
· Exaggerated biceps, triceps, or patellar reflexes
· Brisk or “jumping” responses
· Spread of reflexes to nearby muscles
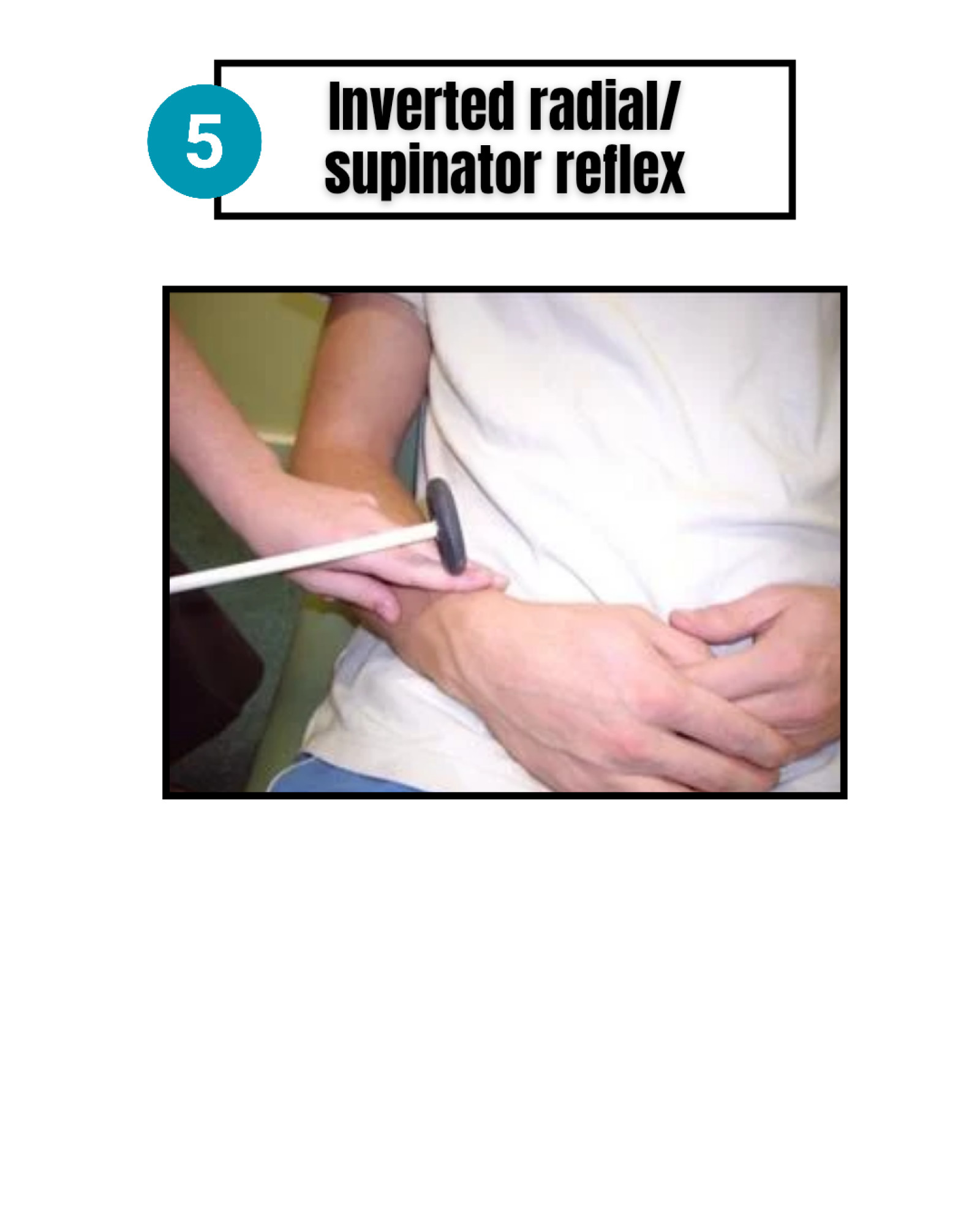
5. Inverted radial/supinator reflex
Positive finding includes:
· Absent or reduced brachioradialis contraction, -Finger flexion occurs instead (an unexpected response)
This “inverted” pattern indicates that:
· The peripheral reflex arc of C5/C6 is not functioning normally
· The finger flexor muscles (C7/C8), controlled by UMN pathways, are overactive
This combination strongly points toward myelopathy, not just radiculopathy.

Managing degenerative cervical myelopathy
Management decisions rely heavily on the severity of symptoms, and one of the most valuable tools for this is the modified Japanese Orthopaedic Association Score (mJOA).
This structured scoring system helps classify DCM into mild, moderate, or severe, guiding whether a patient may benefit more from surgical decompression or supervised conservative care.
Using the mJOA Score to Guide Management
mJOA Score Basics
→ 18 = normal
→ 15–17 = mild DCM
→ 12–14 = moderate DCM
→ ≤11 = severe DCM
International consensus, including recommendations from the ReCODE-DCM group and work by Fehlings et al. uses these cut-offs to guide treatment.
1. Moderate or Severe DCM (mJOA ≤ 14): Surgery is Recommended
For patients scoring 14 or below, evidence suggests that:
· DCM is already impacting spinal cord function significantly.
· Progression is likely without intervention.
· Delays can lead to irreversible damage.
Recommendation:
· These patients should be offered surgical decompression.
· Surgery aims to stop progression and often improves neurological function.
2. Mild DCM (mJOA 15–17): Mixed Approach
This group lies in a grey zone, and decisions should be individualised.
Management Options:
☑ A. Surgical Intervention
· Can prevent deterioration.
· Considered especially for patients showing progressive symptoms.
☑ B. Supervised, Structured Rehabilitation
A trial of:
· Physiotherapy
· Strength and balance training
· Education
· Regular monitoring
Key requirement:
Close, serial follow-up with safety-netting.
If symptoms worsen or fail to improve → reconsider surgical referral.
3. Radiographic Compression Without Symptoms (mJOA 18)
These patients have spinal cord compression on imaging but no symptoms of myelopathy.
Recommendation:
· Do NOT offer prophylactic (preventive) surgery.
· Provide education and safety-netting:
If symptoms emerge → reassess urgently.
4. Radiculopathy With Cord Compression but No Myelopathy (mJOA 18 + Radiculopathy)
This is a commonly encountered group in clinical practice. These patients have a Score 18 (no myelopathy).
· They have radiculopathy (shooting arm pain, segmental weakness).
· They also have cord compression on MRI, meaning they are at higher risk of developing DCM.
Recommendation:
They should be:
· Counselled about the increased risk of progression.
· Offered surgical intervention OR a trial of structured rehab, similar to the “mild DCM” pathway.
If you want to learn more about this topic, you can watch Andy Coombs's lecture here:



