Radiculopathy vs Peripheral Neuropathy: How to Clinically Differentiate
When a patient presents with numbness, tingling, or weakness, the challenge for any clinician is clear: where is the problem coming from? Is it at the nerve root (radiculopathy), or further along the pathway in the peripheral nerve (neuropathy/entrapment)?
Mistaking one for the other can delay recovery and lead to misdirected treatment. That’s why it’s essential to understand the patterns, tests, and clinical reasoning strategies that help differentiate between the two.
If you want to learn more about this topic, you can watch Andy Coombs' lecture here:
What is radiculopathy and peripheral neuropathy?
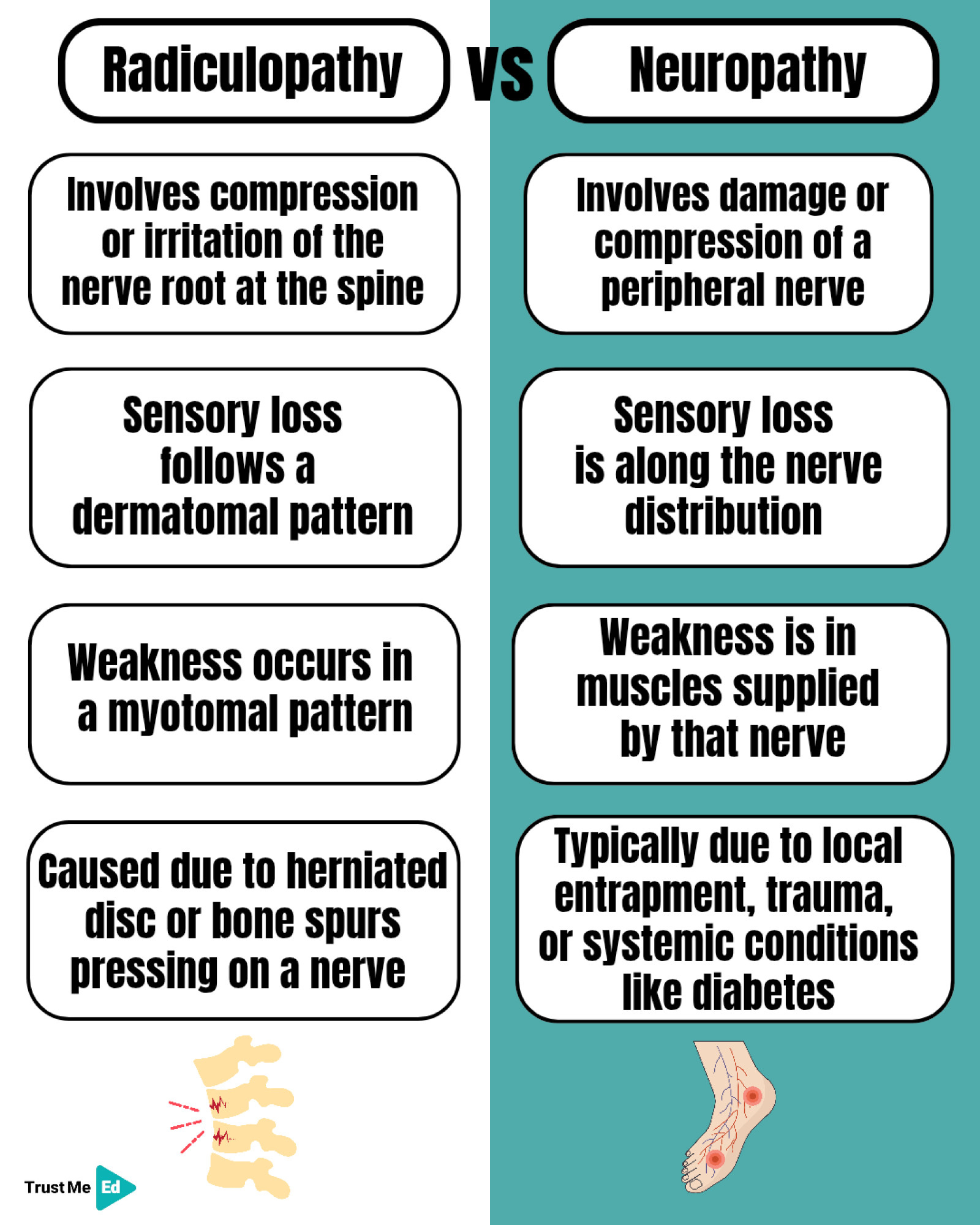
Radiculopathy
A problem at the nerve root (spine) that produces pain, sensory changes, and weakness following a dermatomal or myotomal pattern.
Peripheral Neuropathy
A problem at the peripheral nerve level (e.g., carpal tunnel, cubital tunnel, radial tunnel) that produces deficits following a cutaneous nerve field or specific muscle distribution.
What are clinical clues to tell them apart?
Here are 4 simple but powerful clinical clues to differentiate radiculopathy from peripheral neuropathy:
1. Sensory Patterns
• Radiculopathy → loss follows a dermatome.
• Neuropathy → loss follows a cutaneous nerve field.
2. Motor Patterns
• Radiculopathy → weakness follows a myotome.
• Neuropathy → weakness is localized to specific muscles innervated by the nerve.
3. Reflexes
• Reflex changes can support the diagnosis, but they’re not definitive.
4. Provocation Tests
• Cervical spine maneuvers (e.g., Spurling’s test, distraction test) often provoke radicular symptoms.
• Peripheral nerve tests (e.g., Tinel’s, Phalen’s, Durkan’s) reproduce neuropathic symptoms at entrapment sites.
Key takeaway: Don’t rely on a single test. Always layer your findings — think sensory, motor, reflex, and provocation together.
Peripheral entrapment sites you shouldn’t miss!
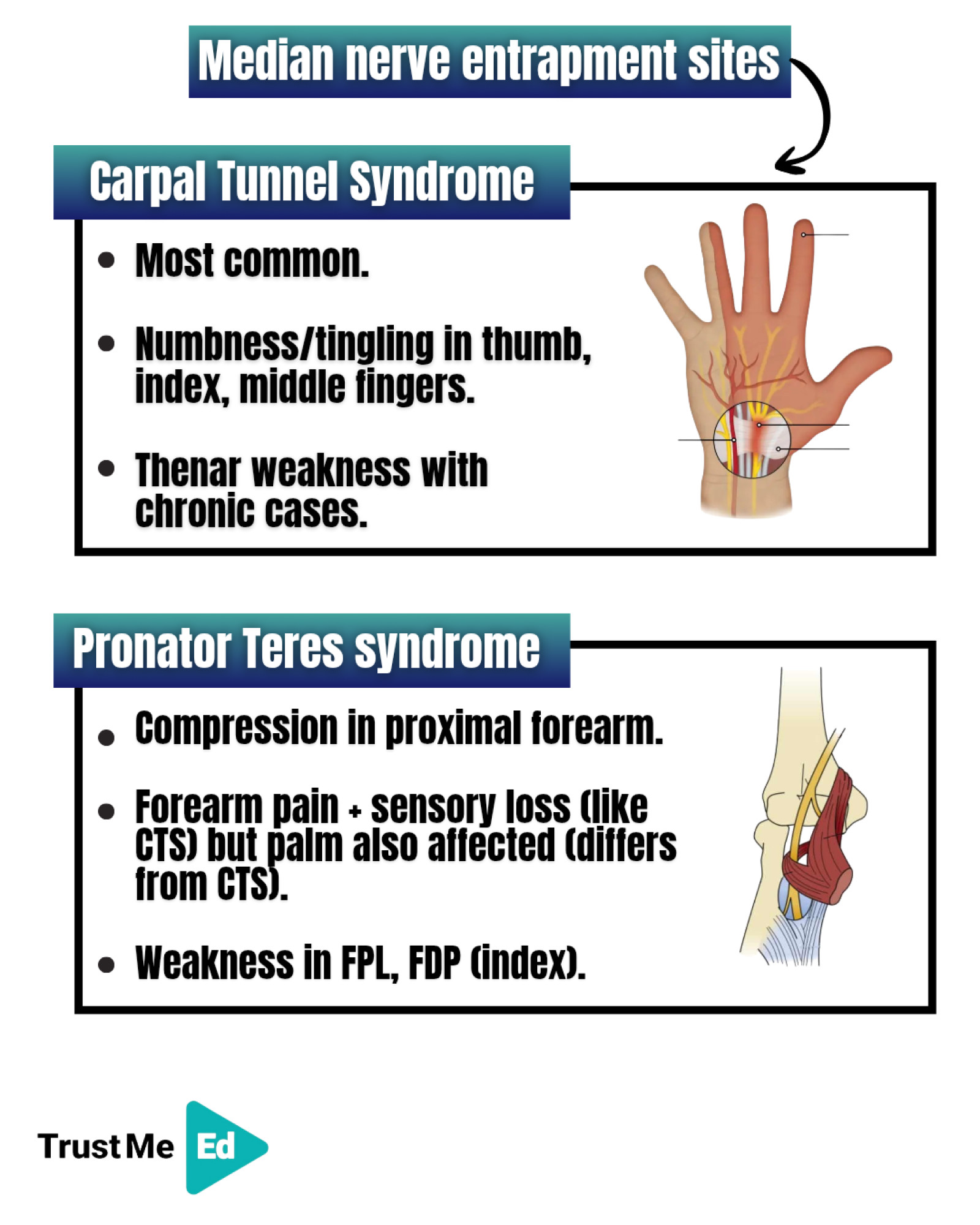
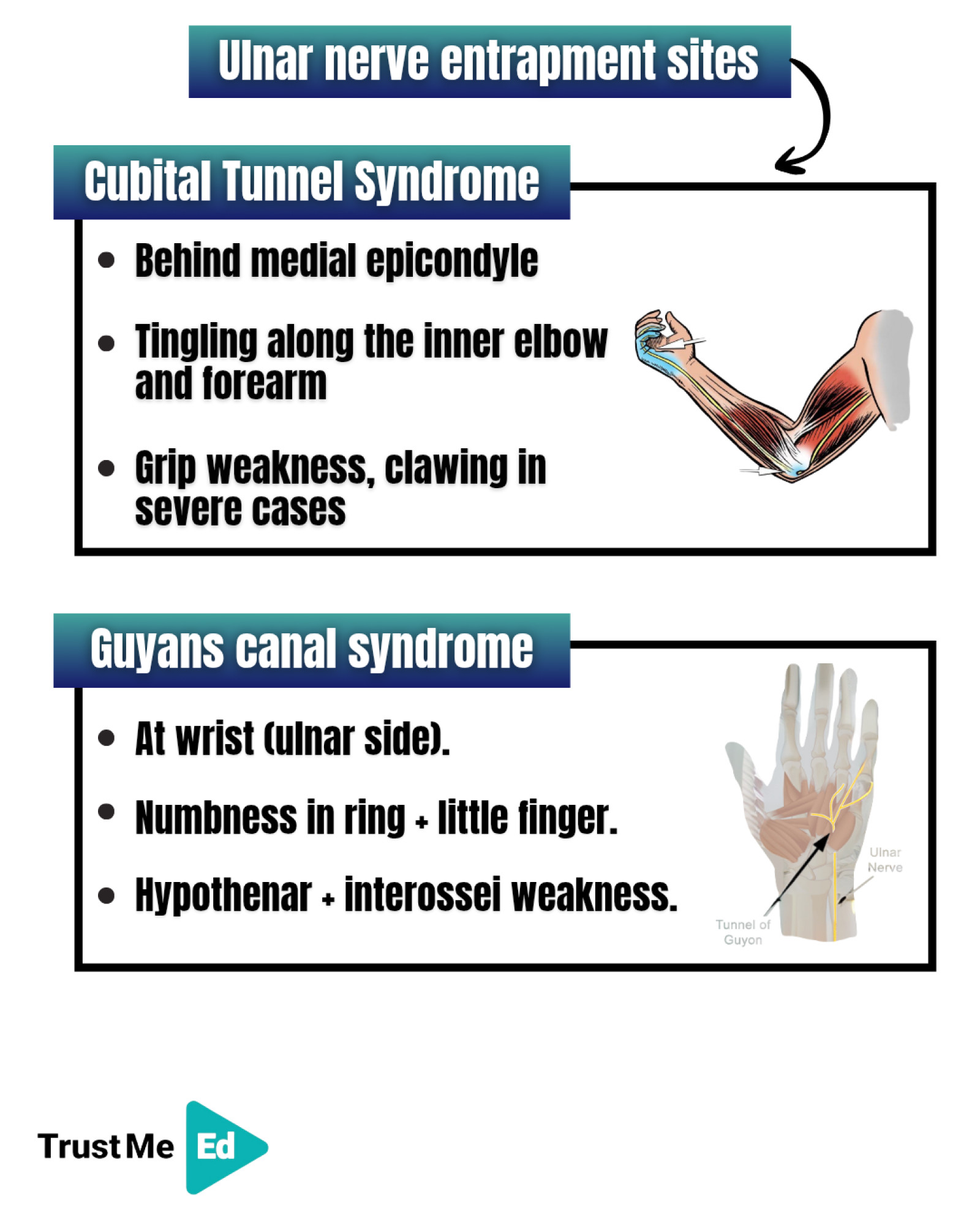
Some of the most common traps for nerves include:
• Median Nerve → Carpal tunnel, Pronator teres.
• Ulnar Nerve → Cubital tunnel, Guyon’s canal.
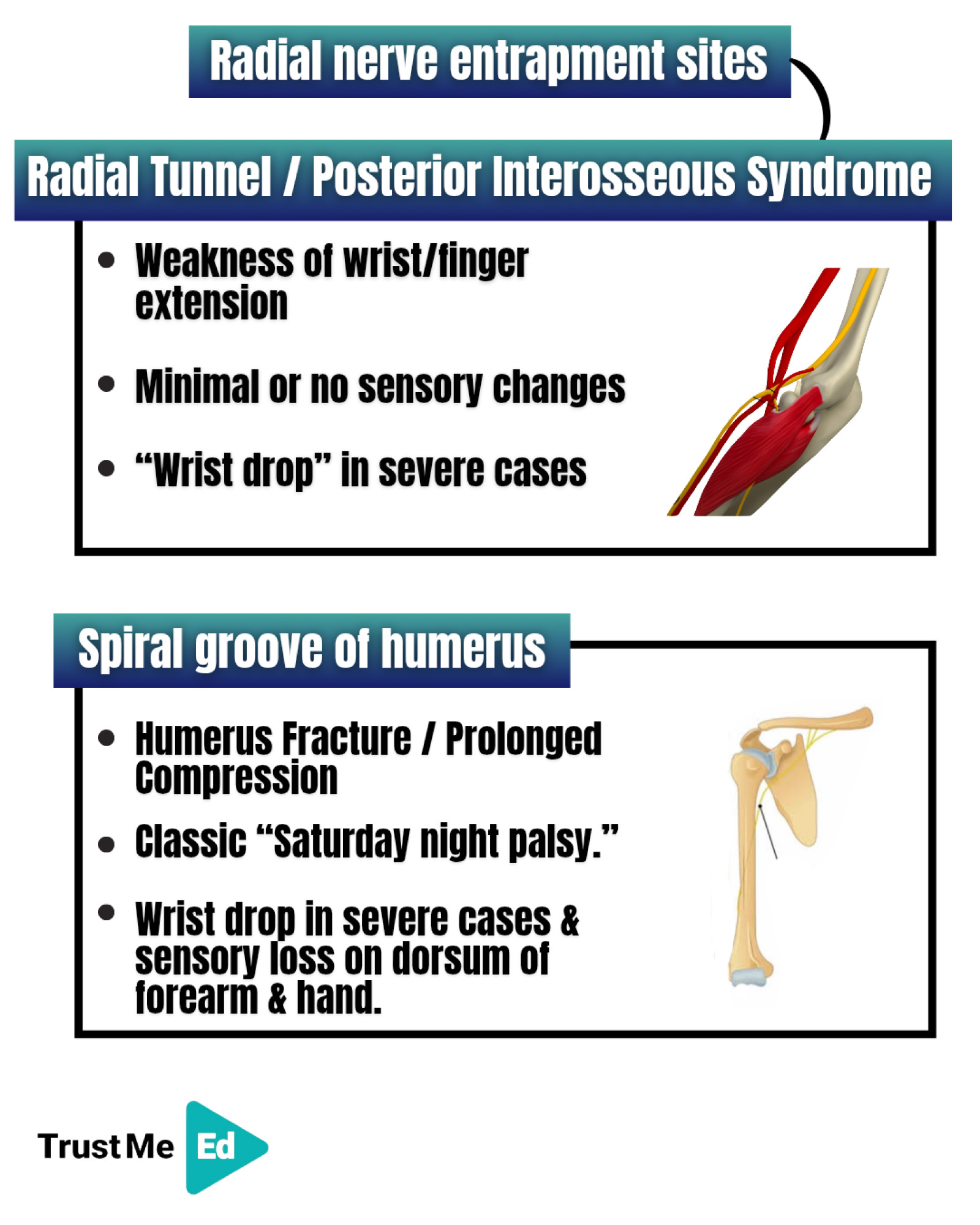
• Radial Nerve → Spiral groove, Supinator (Arcade of Frohse).
Missing these can lead to mislabeling symptoms as “radiculopathy,” when the true culprit is much more distal.


Clinical signs worth knowing:
Sometimes, the diagnosis hides in simple clinical signs:
• Distraction Test → Relief of arm pain when traction is applied to the cervical spine suggests radiculopathy.
• Froment’s Sign → Thumb flexion when gripping paper indicates ulnar nerve weakness (adductor pollicis).
• Wainner’s Cluster → Combining tests (Spurling’s, ULNT1, cervical rotation, distraction) significantly increases diagnostic accuracy for cervical radiculopathy.
Final Takeaway
︙Radiculopathy vs Peripheral Neuropathy isn’t about one test. It’s about recognizing patterns.
︙ By layering sensory, motor, reflex, and provocation findings, you’ll avoid common pitfalls and make sharper clinical decisions.
If you want to learn more about this topic, you can watch Andy Coombs' lecture here:
Source:
1. From the lecture "Clinical Reasoning in Cervical vs Peripheral Neuropathies" by Andy Coombs.



